Child marriages and adolescent pregnancies are becoming rampant in Bangladesh after COVID-19. While tackling these, it’s important to remember Bangladesh’s maternal healthcare system and how it developed over the years.
Maternal death is defined as the death of a woman while pregnant or within 42 days of the termination of pregnancy, regardless of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
0
Maternal Deaths per 100,000 Live Births in 2022
Maternal Death Target to be Achieved by 2030
Less than 70 maternal deaths per 100,000 live births
Neonatal Death Target to be Achieved by 2030
Less than 12 neonatal deaths per 1000 live births
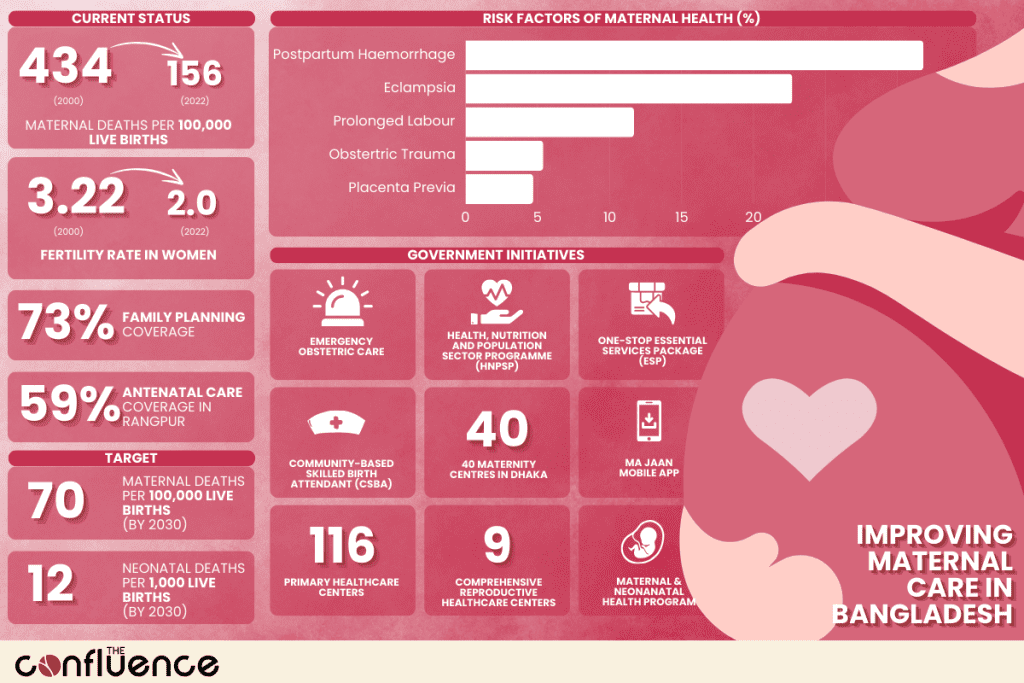
With technological advancements breathing new life into the health and medical sectors, Bangladesh has witnessed a substantial decrease in maternal mortality rates. Bangladesh has made remarkable strides and has emerged as a clear exemplar in reducing neonatal and maternal mortality. However, further efforts are required to achieve the country’s Sustainable Development Goal (SDG) targets of less than 70 maternal deaths per 100,000 live births and 12 neonatal deaths per 1,000 live births by 2030. The maternal mortality ratio, measured as deaths per 100,000 live births, has decreased significantly from 434 in 2000 to 156 in 2022.
Maternal Mortality Ratio in Bangladesh
Source : World Bank (modeled estimate, per 100,000 live births)
No Data Found
Factors Contributing to Risks in Maternal Health in Bangladesh
0
%
Of Child Births Occur before Girls Reach 18 Years Age
54% of Girls
Married before the age of 18
18% of Girls
Married before the age of 15
Child marriage and early unions significantly contribute to maternal mortality rates in Bangladesh, a nation grappling with one of the highest child marriage rates globally. By the age of 18, 58% of girls in Bangladesh are married. On the other hand, 18% married by the age of 15. This practice is particularly prevalent in rural areas. Furthermore, 29% of child births occur before girls reach the age of 18. Despite legislation in 2017 setting the legal marriage age at 18 for women, exceptions still allow child marriages to persist.
Fertility Rate (Births per Woman)
Source: World Bank
No Data Found
Bangladesh’s overall fertility rate has shown a decline, currently standing at 2.13 children per woman. However, this decline is not uniform across all demographics, with rural and impoverished women experiencing higher fertility rates than the national average. Family planning coverage at 73%, leaves a considerable portion of women with an unmet need for contraception, representing 27% of the population. Cultural barriers are worsening the situation, with concerns about societal or religious backlash, partner opposition, and apprehensions regarding contraceptive side effects impeding access to reproductive healthcare nationwide. Moreover, rural people are often dissatisfied after the birth of a female child. This leads to higher fertility rates as well.
0
%
Family Planning Coverage
Efforts to mitigate maternal mortality, such as the government’s community-based skilled birth attendant program, have shown negligible results. The reliance on traditional birth attendants for nearly three-quarters of all deliveries, particularly in rural areas, underscores the challenges in addressing primary postpartum haemorrhage barriers to maternal mortality rate reduction. This situation is worsened by low levels of education and rural residence, which correlate with unskilled deliveries.
Gap between the Wealthiest and the Poorest
Increase in Absolute Gap in Antenatal Care ANC4+
From 25.2% in 1996 to 45.8% in 2018
Increase in Absolute Gap in Facility Based Delivery
From 16.5% in 1996 to 51.6% in 2018
Still equal access to family planning, antenatal care, clean and safe delivery, emergency obstetric care are mostly not satisfactory and so far the facilities available in government health centres are not properly utilised. In 1996, the absolute gap in Antenatal Care ANC4+ coverage between the wealthiest and poorest quintiles was 25.2%, but by 2018 this gap had grown to 45.8%. Regional variation in antenatal care coverage shows more variation than family planning. Rangpur, the division with the highest ANC4+ coverage at 59.2% has coverage rates 1.7 times higher than Sylhet, with 34.6% ANC4+ coverage. Other eastern divisions such as Chittagong and Barisal also have lower ANC4+ coverage rates, suggesting that these could be high-priority regions moving forward. Similar to antenatal care, disparities in facility-based delivery coverage have also widened over time. The absolute gap in facility-based delivery between the wealthiest and poorest quintiles grew from 16.5% in 1996 to 51.6% in 2018.
Workplaces in rural or remote areas may not be expected for health workers to be placed. Moreover, the monitoring system is crucial to give more emphasis in policy as studies reported that double job or private practice of doctors is creating problems in effective maternal health service delivery. The relevant policy is weak in dealing with behaviour of the community such as decision making to participate in clinical setup; for example, establishment of community clinics by the government require more community involvement. One of the reasons is that, often these are influenced by political considerations that are found to be counterproductive. Lack of coordination with UHFWCs at union level was a major obstacle and under-involvement of community groups was found to be an obstacle in functioning of the community clinics.
Critical Insights into Maternal Mortality
According to the 2022 DHIS-2 report, postpartum haemorrhage (PPH) emerged as the leading cause of maternal mortality, accounting for 31.8% of the cases. Eclampsia was responsible for approximately 22.7% of maternal deaths, while prolonged labour accounted for 11.7%. Other obstetric traumas, including uterine rupture, contributed to 5.4% of deaths, and placenta previa was the cause of 4.7%.
Place of Death
About 21.7% of maternal deaths occurred at home, and 21.2% happened while en route to healthcare facilities. The remaining cases took place in health facilities.
Place of Maternal Death
Percentage
No Data Found
Postpartam Period
Approximately 64.2% of maternal deaths occurred within 42 days postpartum, 23% during delivery, and 12.8% during pregnancy.
Time of Maternal Death
Percentage
No Data Found
Gestation Period
The majority of maternal deaths (47.8%) occurred between 37 and 39 weeks of gestation. Around 25.2% took place between 33 and 36 weeks, and 6.3% occurred within 28 weeks of gestation.
Time of Maternal Death
Percentage
No Data Found
Antenatal Care
About 34.9% of mothers had four or more antenatal care (ANC) visits before their death. While 86% attended at least one ANC visit, 77.2% made two visits, and 64% had three visits. Approximately 14% of mothers did not attend any ANC visit before their death.
Postnatal Care
Around 52.3% of mothers did not receive any postnatal care (PNC) before their death. Approximately 47.7% had only one PNC visit, and 28.5% had two PNC visits before their death.
Type of Delivery
Approximately 70% of the deliveries were normal vaginal deliveries (NVD), while caesarean sections were performed in 29% of the cases.
Steps Taken to Promote Maternal Health
Introduction to New Approaches
During the 1990s, the emergency obstetric care (EmOC) approach gained prominence in Bangladesh, supported by international organisations like UNICEF, UNFPA, and the Averting Maternal Death and Disability programme. These initiatives focused on renovating and upgrading existing healthcare facilities and training staff to provide emergency obstetric care.
With the development of the National Maternal Health Strategy in early 2000s, the approach broadened, incorporating a rights-based approach to safer motherhood. This strategy was integrated into the ongoing Health and Population Sector Programme (HPSP) and subsequently the Health, Nutrition and Population Sector Programme (HNPSP), which outlined the policies and programs for government healthcare services.
The delivery of interventions was streamlined through the one-stop essential services package (ESP) at the primary healthcare level, where health and family planning cadres were unified under a single management structure. Among the five components of the ESP, maternal health was given the highest priority, with a focus on EmOC to reduce maternal mortality and basic obstetric care for promoting good practices, early detection of complications, and appropriate referrals.
The Bangladesh Maternal Health Strategy recommended a community-based skilled birth attendant (CSBA) strategy to complement the facility-based approach. The strategy set a target of one six-month-trained CSBA for every 6,000-8,000 people. The Obstetrical and Gynaecological Society of Bangladesh, in collaboration with the Ministry of Health and Family Welfare (MoHFW), WHO, and UNFPA, initiated a pilot project in 2001 to train existing Family Welfare Assistants (FWAs) and female Health Assistants (HAs) to provide antenatal care, basic emergency obstetric care, postnatal care, and essential newborn care at the household level.
The CSBA training program was gradually expanded to 28 of the 64 districts in the country. By June 2007, approximately 2,500 FWAs and female HAs had completed their training and were deployed to provide home-based skilled delivery care, in addition to their previous family planning responsibilities.
Project to Aid Emergency Obstetric and Newborn Care
0
Maternity Centers in Dhaka
The ‘Solving Referral Challenges for Urban Poor to Access Emergency Obstetric and Newborn Care’ project was launched in June 2020. Funded by UNFPA and operated by BRAC through 40 maternity centres in Dhaka, this initiative uses an app called ‘Ma Jaan’ to connect pregnant women in emergencies to the nearest hospital associated with the project. The project has been successful, serving as a concrete example of using technology to prevent maternal deaths during pregnancy, delivery, and postnatal complications.
Second Urban Primary Health Care Project
0
Primary Healthcare Centers
To address high levels of child and maternal ill-health, the Second Urban Primary Health Care Project was implemented from 2005 to 2011. This initiative aimed to improve the health status of the urban population, particularly the poor, across six city corporations and five identified municipalities. The project focused on delivering a comprehensive package of preventive, promotive, and curative health services, with at least 30% of these services targeted at the poor.
The project operated through public-private partnerships. The Asian Development Bank (ADB) primarily financed the project, with co-financing from the Department for International Development (DFID) of the United Kingdom, the Swedish International Development Cooperation Agency (SIDA), and the United Nations Population Fund (UNFPA).
As part of this project, 116 primary healthcare centres and 9 comprehensive reproductive healthcare centres were established.
Health Population and Nutrition Sector Development Program
To accelerate progress in the health, population, and nutrition (HPN) sector and address its challenges, the Ministry of Health and Family Welfare (MOHFW) of the Government of Bangladesh (GOB) implemented the Health Population and Nutrition Sector Development Program (HPNSDP). This program ran for five years, from July 2011 to June 2016. As a result of this program, there were significant declines in the maternal mortality ratio, infant mortality rate, and under-five mortality rate. Additionally, the population growth rate and total fertility rate (TFR) decreased, while the percentage of children receiving vitamin-A supplements and life expectancy at birth increased. The total estimated cost for this program was Tk 569.9 billion.
As an extension of this project, the MOHFW initiated the development of a pilot model for Zero Maternal Deaths in Moulvibazar, Sylhet, in collaboration with various NGOs. This model aimed to track every pregnancy using IT services, equip facilities with necessary resources, develop the capacity of service providers for effective implementation, and execute a joint monitoring plan. The timeline for this pilot project was 2019-2022. Organisations such as UNICEF, UNFPA, Save the Children International (SCI), BRAC, CIPRB, OGSB, BNF, BPA, and ICDDR,B contributed to this project.
Update in Labour Room Protocol
In response to the COVID-19 pandemic, OGSB Maternity Hospital, with technical assistance from UNFPA and ICDDR,B, has updated its Labour Room Protocol. This protocol governs the management of women during labour amidst the COVID-19 crisis. Standard guidelines have been established for patients attending the Antenatal Clinic, Labor and Delivery Ward, and Postpartum Clinics. The updated protocol addresses the care of pregnant women, managing both normal and low-risk labour, as well as abnormal and high-risk labour.
Additionally, the protocol incorporates an infection prevention and control program, including the use of personal protective equipment (PPE), to mitigate the risk of infection among healthcare providers and patients. This ensures the continuity of care in a safe environment.
Maternal and Newborn Health Service Accreditation Program
The Maternal and Neonatal Health (MNH) Service Accreditation Program in Bangladesh was initiated in 2020 with the goal of developing a robust accreditation system for health services aimed at improving the quality of care (QOC). This initiative is led by the Health Services Management (HSM) and the Directorate General of Health Services (DGHS) under the piloting approach of the Primary Health Care and Family Planning (PHCFR) and Accreditation component of HSM’s Operational Plan. The DGHS serves as the awarding body for this accreditation.
Technical support, capacity building, and operational support for piloting the Service Accreditation for MNH services have been provided by USAID’s MaMoni Maternal and Newborn Care Strengthening Project (MNCSP). This program is designed to ensure the provision of quality MNH care in both public and private facilities, covering three critical dimensions: value for facility, value for patients, and value for the healthcare system.
Value for Facility
The value for the facility ensures a minimum set of standards for MNH services, facilitates standardised work procedures, and promotes the delivery of respectful maternity care.
Value for Patients
On the other hand, value for patients enhances the overall experience of care, provides better quality care, leading to improved health outcomes for women and newborns, and ensures safer and more respectful care. It aims to increase patient satisfaction.
Value for Healthcare System
The value for the healthcare system guarantees that certified or accredited facilities adhere to national quality standards for MNH care and aligns with national MNH priorities and the Sustainable Development Goals (SDGs).
Initiatives By CARE Bangladesh
CARE International, an NGO, has launched various programs to enhance maternal health in Bangladesh, including the Joint Action for Nutrition Outcome (JANO). This program educates mothers and pregnant women about health issues, nutrition, and precautions during and after pregnancy, reshaping their understanding of the importance of accessing professional health care services.
Another initiative by CARE, the SHOUHARDO III program, has also made significant strides in enhancing maternal health in Bangladesh. In 2021, this program trained female private community skilled birth attendants to assist pregnant and lactating women in the remote Char and Haor areas of northern Bangladesh. These trained professionals provide safe delivery services, antenatal and postnatal checkups, counselling, and referrals.
Strengthening the Maternal and Neonatal Health System
Save the Children has announced the launch of a five-year project titled “Strengthening the Maternal and Neonatal Health System in Rangpur,” with a budget of $10 million. This project will be implemented from March 1, 2023 to December 31, 2027. Funded by the government of the Republic of Korea through the Korea International Cooperation Agency (KOICA), the project is a collaboration between Save the Children Bangladesh and Save the Children Korea under the KOICA-NGO partnership.
The project aims to reduce the maternal mortality ratio in the Rangpur division by increasing the utilisation of healthcare services. The project will initially focus on the Rangpur and Lalmonirhat districts, with implementation occurring in three phases. The first phase, covering the next five years, will concentrate on Rangpur and Lalmonirhat. The results and progress from phase one will guide the subsequent expansion to the remaining districts in phases two and three.
Establishment of Maternity Hospitals
In March 2023, the Ministry of Health announced plans to establish 30 to 50 bed maternity hospitals, also known as mother and child hospitals, in every district across the country. This initiative aims to reduce pregnancy-related complications and lower healthcare costs.
To date, the government has established 14,000 community clinics, which now offer 32 types of healthcare services and medicines to people in rural areas. By October 2022, the government had launched 500 Model Union Health and Family Welfare Centres nationwide as part of its efforts to reduce maternal and newborn mortality rates. These health centres throughout the country have already implemented 24-hour healthcare services for pregnant mothers.
0
Target of the number of midwives by 2026
In addition, the government has established 5,500 Health and Family Welfare Centers at the union level to reach every mother and child in the country. To provide 24/7 services to pregnant women, the government is planning to deploy four midwives at each of these centres. Additionally, the government is working to increase the total number of midwives to 20,000 by 2026.
The public sector health service delivery system is divided into primary, secondary, and tertiary levels. At all levels, maternal and child healthcare is prioritised in policy and implementation to achieve the Sustainable Development Goals (SDG) targets.
The Safe Motherhood Promotion Project
The Safe Motherhood Promotion Project (SMPP) was launched in July 2006 by the Ministry of Health and Family Welfare (MoHFW) with support from the Japan International Cooperation Agency (JICA) as a technical partner. The primary goal of this initiative was to enhance the health status of pregnant and postpartum women, as well as neonates, in the Narsingdi district. Due to the success of its maternal and neonatal health interventions at both community and health facility levels, SMPP became known as the “Narsingdi Model.”
Following the completion of the initial five-year phase, the second phase of the SMPP project commenced in July 2011. This phase aimed to consolidate and expand the effective practices established during the first phase, with the objective of improving the quality and utilisation of maternal and neonatal health services across Bangladesh. SMPP-2, also a five-year project, operates at the national policy and decision-making levels and includes interventions in Satkhira, Jessore, and Narsingdi districts. The activities of SMPP-2 encompass several key areas including scaling up of good practices, quality improvement of hospital services, revitalization of community clinics and community support groups, introduction of a maternal and neonatal health intervention package under the Upazila Health System, engagement of local government etc.
Bangladesh National Strategy for Maternal Health
85% Institutional Delivery
Targeted within 2030
90% Delivery Attended by Skilled Attendants
Targeted within 2030
4 Antenatal and Postnatal Care
Within 48 Hours
85% Contraceptive Prevalence Rate
Targeted in the National Strategy
The primary objective of the Bangladesh National Strategy for Maternal Health (2019-2030) is to expedite the reduction of maternal and neonatal mortality and to alleviate the burden of maternal and neonatal morbidity. To accomplish this, the strategy focuses on ensuring that skilled attendants are available at every birth and that the majority of women have equitable access to quality delivery care in well-equipped and adequately staffed health facilities. By 2030, this strategy aims to have 85% of institutional delivery, 90% of deliveries attended by skilled birth attendants, at least four antenatal care and postnatal care within 48 hours from a medically trained provider for all. This strategy aims to increase the contraceptive prevalence rate by 85% as well.
The Way Forward
The GoB should strengthen primary healthcare infrastructure in rural and underserved areas. Upgrading and equipping existing healthcare facilities with adequate supplies, equipment, and skilled personnel can contribute to changing the situation. Moreover, improved transportation and referral systems for timely transfer of complicated cases is necessary.
Scaling up community-based skilled birth attendant (CSBA) training programs can help to reduce maternal mortality rate. Providing incentives can help to retain skilled birth attendants, especially in rural areas.
Cultural barriers play a huge role in maternal mortality. Implementing comprehensive awareness and education campaigns to address cultural barriers and misconceptions can help to reduce these existing misconceptions.
Increasing availability and accessibility of modern contraceptive methods can reduce maternity related health issues to a great extent. Providing counselling and education on family planning options is necessary. In this regard, targeted interventions for high-risk groups like adolescents, low-income women, and regions with poor indicators can accelerate the initiative .
The GoB should enforce and strengthen laws and policies to prevent child marriage and adolescent pregnancies.
Establishing robust monitoring and evaluation systems for maternal health programs will improve accountability mechanisms for healthcare providers and facilities.
The Government should foster partnerships with NGOs, community-based organizations, and international agencies.
About the Author

Umme Farzana Rupa, a former debater, currently excelling as a passionate student at Bangladesh University of Professionals. Engaging communicator and dedicated learner, she continues to thrive in academics, leaving her mark on campus with her inquisitive spirit and determination.