Bangladesh is committed to ensure ‘Health for All’-a declaration of the Alma-Ata made on Primary Health Care (PHC) that was unanimously adopted by the member states in 1978. With this in view, in 1998, community clinics were introduced in Bangladesh as a wider approach to health care for every individual of the country. The Mission has been said to play a key role in global health diplomacy. Has the establishment of community clinics really revolutionized the health sector? How was the outlook of the whole world on this initiative?
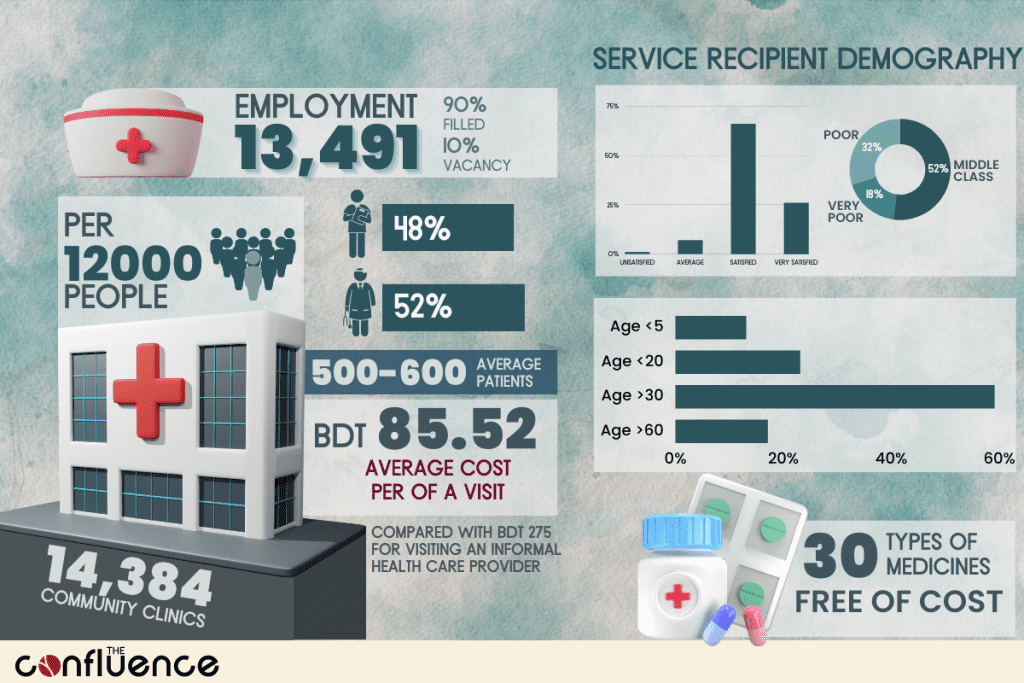
Bangladesh aims to provide the right to access quality healthcare without facing financial hardship to all citizens to achieve Sustainable Development Goals (SDG) and Universal Healthcare Coverage (UHC). As a part of its existing primary health care system, the government of Bangladesh in 1998 started to establish Community Clinics (CC), one CC for roughly each 10,000 people in rural Bangladesh. By 2001, the physical infrastructure of 10,723 clinics was constructed and approximately 8,000 community clinics were operational. The original project was later thwarted following a regime change in 2001, which was later revived under the Revitalization of Community Health Care Initiatives in Bangladesh (RCHCIB) project in 2009. The Ministry of Health and Family Welfare (MoHFW)’s Community Based Health Care Operational Plan (June 2011-2016) aimed to establish 13500 Community Clinics (CC) within June 2016. Up to 30 September 2017, a total of 13 442 CCs were reported to be in operation. According to the Finance Minister’s budget speech in June 2023, there are a total of 14,384 community clinics as of FY 2022-23, in current estimates of population, this amounts to one CC for each 12000 people. However, according to the Facility Registry of MoHFW, a total of 14114 CCs were reported.
0
Community Clinics
Community Clinic turns the concept of public-private-partnership into reality as all Community Clinics are constructed on lands donated by people of the community being served; costs relating to construction, medicines, and all necessary logistics, salaries of service providers are met from the government revenues and development funds but the management is borne by the community people.
0
people covered by one community clinic
Each Community Clinic is headed by a Community Healthcare Provider (CHCP) who works 6 days a week; a Health Assistant (HA) and a Family Welfare Assistant (FWA) who work alternatively 3 days a week. A Community Group (CG) that is pivotal in the management of CC consisting of 13–17 members, headed by the elected Union Parishad (UP) Member manages the CC. In the catchment area of each CC, there are three Community Support Groups (CSGs) each comprising 13–17 members.
Impact of Community Clinics in Attaining Universal Healthcare Coverage (UHC)
Since inception, community clinics have been playing an epoch-making role in improving the overall antenatal and postnatal care, family planning and nutritional services, providing treatment for diarrhea, pneumonia and other childhood infections and counseling on the consequences of early marriage in Bangladesh. With the integration of ‘Community Clinic Health Assistance Trust Act, 2018’, millions of people are getting services from the community clinics whereas just a decade ago healthcare facilities in the rural areas were very poor.
500-600 Average Visitors
Per Community Clinic Per Month
Community health centers offer low-cost healthcare services such as dental, medical, and behavioral healthcare. Studies estimate that the provision of care in community health centers ultimately saves the central health care system an impressive amount of money annually by eliminating unnecessary emergency room visits and other hospital-based care. There is no denying that community clinics are essential in Bangladesh as they promote accessibility and affordability of healthcare services, particularly in rural areas. They contribute to disease prevention, early intervention, and health education, ultimately leading to improved health outcomes and a stronger healthcare system. According to a survey conducted in 2016 by ICDDR,B the formation of Community Support Groups (CSGs) for expectant mothers, receiving antenatal care increased to 84% after forming CSGs compared to 69.6% before forming them. The CSG based community support system can play a significant role in improving healthcare if implemented at a large scale.
0
Types of Medicines Provided for Free
Community Clinic Services
Primary healthcare in all areas and distribution of free medicines
Counseling services
Regular checkups, advice and free medicines for pregnant women
Immunization against contagious diseases for children
Safe delivery using modern methods
Health counseling for adolescents
Health services for aged
Family planning services
Nutrition advice
Primary emergency services
Awareness of disease prevention
Integrated Management of Childhood illness
Other than the aforementioned services, community clinics provide free/subsidized medicine to the underprivileged population. A total of 30 types of medicines are provided free of charge to the underprivileged population in the rural or peripheral areas including medicine for hypertension and diabetes.
Average Cost of Visit
BDT Per Visit
No Data Found
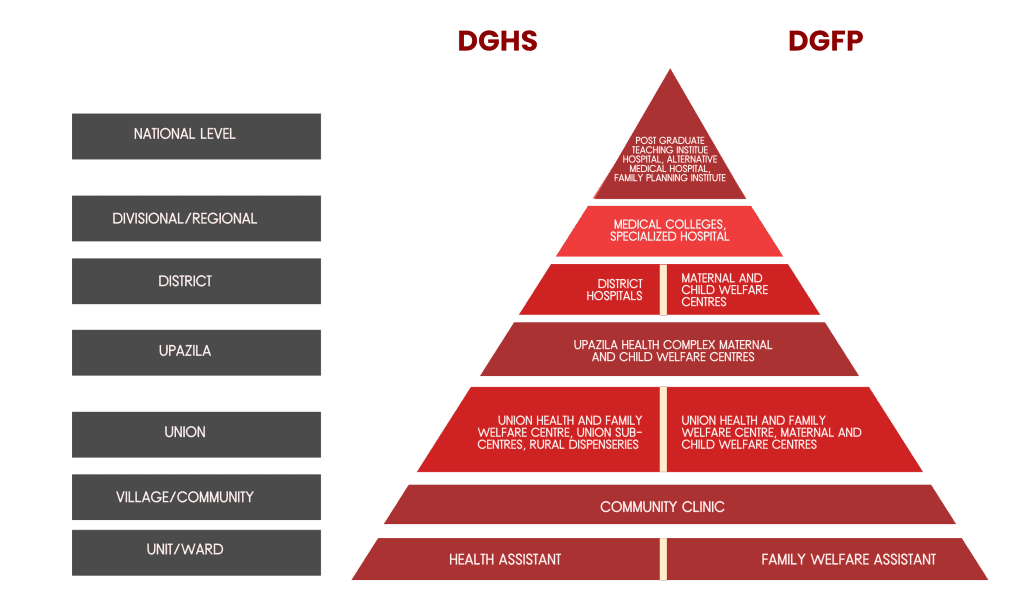
The First Step towards Referral System
Bangladesh’s healthcare system suffers from inadequacy of healthcare professionals. However, the problem is made even worse without a proper referral system. There is a service demand and service availability mismatch. In absence of a referral system, people suffering from minor health issues tend to visit a specialist, increasing the demand of specialists even if specialist consultation is not needed. Thus exhausting the already limited expert availability. Without a multi-level healthcare facility in place, it would be difficult to ensure healthcare in the periphery as well as maintain a bottom-up referral system. With community clinics in the most peripheral parts of the country, it is easier to refer patients with serious issues to upazila or district level hospitals and to divisional/regional and national level hospitals thereafter.
Multilateral Cooperation of the Government and Development Partners
The revitalization of community clinics required huge investment, mostly fixed investments to set up the facilities and hard infrastructure etc. The Government and the Development Partners (PA) like JICA, WHO, GAVI, HSS, USAID and others provided the necessary funding. As per previous analysis, development aid has helped Bangladesh achieve major goals in the healthcare sector particularly. However, the project aids come in two models –
1. Direct Project Aid (DPA)
The aid is directly provided to the government for implementation of a project according to its merit.
2. Reimbursable Project Aid (RPA)
The government has to bear the expenses first, upon obtaining a satisfactory level of outcome, the development partners reimburse the expenses previously incurred.
After analyzing the National Operational Plan for Community Based Health Care, a breakdown of estimated costs show that 24.9% of the total estimated cost was supposed to be borne by the government directly. The lion’s share of 41.2% was supposed to be initially borne by the government as reimbursable project aid (RPA) to be reimbursed by the development partners upon achieving satisfactory results from the project. And another 33.7% of the costs came as direct project aid (DPA). Since, RPA has already been spent on the project by the government, it is important to attain the projected outcome in order to get the project aid reimbursed.
% of Total Expenses
No Data Found
On the other hand, MoU has been signed with eight NGOs to work with the government to develop the capacity of CG and CSG, involve the community, and conduct some operational research on CC. GAVI-HSS is supporting the development of CG and CSG’s capacity to establish solar panels, renovate for MNH services, including the ability to conduct normal deliveries at CCs, and engage in many other CC activities.
https://youtu.be/pndal8AWy_I
Public Satisfaction and Appraisal
According to an assessment published by the Implementation, Monitoring, and Evaluation Division (IMED) of the Planning Ministry in 2014, 82% of the people of various localities avail the services of the community clinics. The assessment further showed that an average of 35 persons visit the clinics each day. Due to the proximity of the clinics to peoples’ homes and provision of free medicines for common ailments, the number of people visiting the clinics is on an increase.
Two other studies also corroborate the findings about public confidence in these clinics. A survey of the National Institute for Population Research and Training (NIPORT) shows that 80% of the people are satisfied with the medicines and advice from the clinics. The National Institute of Preventive and Social Medicine (NIPSOM) showed that 98% of people are satisfied with the services.
In February 2018, WHO Bangladesh commissioned the hera–HAL consortium to conduct an independent evaluation of the CBHC programme in Bangladesh. According to the evaluation report, the reported number of visits to CC for services increased by 57% from 2014 to 2017.
Total number of
community clinic users
by year 2014-2017
- 201455561652
- 201584702755
- 201686877640
- 201788234600
The people interviewed mentioned a number of hurdles to accessing CC services, including a lack of transportation, bad roads, living in remote places, as well as social and religious barriers. The majority of users (90%) resided locally, suggesting that geographic barriers to accessing CC services may not exist for those who live close by, but may exist for those who live farther away, especially in isolated places. All age categories were represented among the users, with the majority (42%) being between the ages of 30-59; 20% being under 20; 17% being over 60; and 10% being under five. All income quintiles were represented, with nearly half (48%) falling into the poor or extremely poor category. More than seven in ten users (77%) were female. Only 7% of the users had completed higher secondary education or above, indicating that most recipients of healthcare services at the community clinics were less educated. While the demand for promotional and preventative services was low during the evaluation period, curative therapies made up the majority of the services provided by CCs (86%).
Gender Profile (%)
of every 100 Community Clinic Users
No Data Found
Gender Profile (%)
of every 100 Community Healthcare Provider
No Data Found
Age Profile (%)
of every 100 Community Clinic Users
No Data Found
Education Profile
of every 100 Community Clinic Users
No Data Found
Perceived Socioeconomic Status of Community Clinic Users
of every 100 people (%)
No Data Found
However, human resources at the CCs need improvement. As per the evaluation report of WHO,tThe shortage and part-time presence of HAs and FWAs hinders the availability and continuity of services at the CC since HAs and FWAs are supposed to work on alternate days according to the original plan. In terms of establishment of a referral system, although there are clear procedures for referring patients from CCs to higher level facilities, the next level of the health system, Union Facility is frequently skipped over and patients are sent directly to the Upazila Health Centers.. Counter-referrals and feedback were not done in a systematic way. By adding the case as a unique ID and referring to a higher institution, the current referral system should be reinforced.
0
Cost-Benefit Ratio
which implied that BDT 100 (USD 1.19) investment in CCs generated a benefit of BDT 123
The average cost of a patient to visit a CC (excluding family planning) was BDT 85.52; significantly lower than the BDT 275 cost of visiting an informal health care provider. The cost-benefit analysis (CBA) findings demonstrated that all accruing advantages exceeded all expenditures, resulting in a net benefit of BDT 1511.51 million (USD 18.00 million) that was sizable. The benefit-cost ratio was 1.23, meaning that an investment of BDT 100 in CCs resulted in a benefit of BDT 123, which was greater than any benefit from a traditional investment. The provision of high-quality services, the availability of equipment and medications, the development of staff competencies and skills through frequent contact, the regular availability of the provider, the maintenance of an adequate supply of medication and supplies, and the proper maintenance of the equipment are all requirements for receiving this return.
0
Sanctioned Posts
0
Posts filled
10% of Community Healthcare Provider posts are empty
However, in terms of patient satisfaction with services received at community clinics, 26% of the recipients were very satisfied while 66% were satisfied, 7% reported average service and 1% were unsatisfied.
Client Satisfaction with Services Received at Community Clinics
As percentage
No Data Found
However, the evaluation report of WHO concluded that the Community Based Health Care (CBHC) concept is well developed, but implementation puts a greater focus on curative services than preventive and promotive services for the catchment population. In order to fully embrace responsibility for the health, population, and nutrition of the entire catchment area’s population and to carry out its work from a public health and health systems viewpoint, the CC, as the first level static health facility of the CBHC method, must have a proactive rather than a reactive approach (mostly providing curative care for minor ailments of older customers), which calls for analyzing the health condition, recognizing the catchment population, and altering measures to prevent and deal with health problems.
This can be attained by creating a unique ID for the service recipients. In Bangladesh’s case, Smart Cards/NID can have a linked healthcare database. Greater cooperation between the Ministry of Home Affairs and the Directorate General of Healthcare Services (DGHS)’s MIS can ensure further digitalization of the healthcare system of Bangladesh.
Steps taken by the Government on Sector Wide Approach
The implementation period of the Revitalization of Community Health Care Initiatives in Bangladesh (RCHCIB) project is from 1st July 2009 to 30th June 2014. Since then the initiative on Community-based primary health care has been grossly focusing on the following issues :
- Measuring health outcomes
- Staffing and Supervision of Community Clinics
- Proper Community engagement
- Adequate Knowledge about the Referral system
- Sustaining institutionalization
- Upazila Health System
- Medical Waste management
- Tribal Health
- Urban Health
Government Policies have already been taken to ensure proper healthcare for all with the community clinics. Alongside these focus areas, government orders have been made to ensure proper monitoring and supervision of Community Clinics by every individual of Divisional, District and Upazila Level of the Ministry of Health & Family Welfare every month.
Recognition of Community Clinics
The idea of community clinics to ensure ‘healthcare for all’ received widespread recognition. The clinics are now seen as a successful example of primary healthcare and are being adopted by other developing nations. In 2014, the World Health Organization (WHO) released a book named “Community Clinic-Health Revolution in Bangladesh” that detailed the achievements of these clinics. The effort was hailed as a “Bangladesh model for ensuring universal healthcare” during the 68th World Health Assembly of the WHO in Geneva, Switzerland in May 2015.
The resolution titled “Community-based primary health care: a participatory and inclusive approach to universal health coverage,” was termed as “The Sheikh Hasina Initiative’‘ at the United Nations (UN). The proposal ‘Sheikh Hasina Initiative’ was adopted at the United Nations (UN) on 16 May (17 May Bangladesh time) which is coincidentally the homecoming day of Sheikh Hasina. It reflects Bangladesh’s commitment to improve the health and well-being of its citizens and to contributing to global health equity. The resolution was co-sponsored by 70 member states of the United Nations in strong support for community clinic-based health systems.
Limitations to achieve “Health for All” with Community Clinics
- Although the clinics are well located in terms of access, there remains a serious concern that one third are on boggy ground that is subjected to flooding. The objective of all people being within 30 minutes walk has not been fully achieved.
- Most of the buildings conform to the guidance except in the provision of toilets and safe water. The quality of the building varied and about one-quarter showed serious signs of poor workmanship. It is clear that there has not been adequate supervision of some of the development and construction. To some extent this is probably due to the late and unsatisfactory degree of community participation.
- The role of health workers in the clinics requires a wide range of skills and their job descriptions are currently beyond the skill levels of most staff.
- There are some shortages of equipment and furnishings but the main problem is the inadequate and intermittent supply of drugs.
Recommendations
Since its inception, the CC system went through several changes. But it is yet to achieve the desired goal. However, based on findings some recommendations could be forwarded as per expectations of the rural people to enhance the service standards:
- CHCP should be presented at CC on a regular basis. He/she should be provided comprehensive training to carry out his/her responsibilities properly. Thus, comprehensive training should be emphasized.
- The monitoring system should be strengthened including the participation of CGs and CSGs. Involvement of local government on health issues can play a vibrant role in this regard. Certain discretion can be delegated to the local government for effective monitoring.
- Availability of essential drugs must be assured. Supply of medicine should be maintained properly. Also, medicine for varied diseases should be made available to all, particularly to the poorest of the poor. Preferential treatment for particular groups such as CG and CSG members should be checked.
- Besides the government, CGs can play a significant role to make CC accountable. In practice,CGs are not as active as expected. In this regard, CGs should be made more dynamic and active; at least meetings should be conducted on a regular basis with participation of the majority of the members. Moreover, the role of CSGs should be strengthened so that they can contribute to CGs operation.
- Besides CHCPs, other service providers such as HA/FWA should visit CCs regularly. To make advanced treatment accessible to elderly poor, provision should be made for visiting one of the specialized doctors at CC periodically.
- It’s now the demand for all to make e-health service available and accessible. In this regard,the government is very kind to ensure such arrangements and intends to equip all CCs with modern facilities. But using a unique ID for all service recipients and their digital track record to be found in the national database accessible by the doctors can be a way to go about.
- Involvement of government health educators can empower community people. Community Empowerment will be further strengthened if health communications are promoted. More health personnel need to be engaged in health planning.
- Prime Minister Sheikh Hasina has announced the formation of a trust fund for the sustaining the successes of community clinics in the future. The objective to establish such a fund is to give a solid ground for the community clinics across the county and make them self-reliant so that no one could shut these down after the change of government. The establishment of such a trust fund for long-term sustainability has to be realized.
- To the broader extent, health and FP dichotomy should be checked so that proper coordination can take place.
About the Author
The Bangladesh Medical Students’ Society (BMSS) is a national member organization of the International Federation of Medical Students Association (IFMSA). IFMSA is an entity recognized by the World Medical Association, World Health Organization, and United Nations as the global voice of medical students.